Understanding the Mechanisms Behind Blocked Arteries in the Heart
Exploring the Process of Atherosclerosis and its Impact on Heart Health
Have you ever wondered how arteries, the very vessels that keep our heart ticking, can become blocked? It’s a bit like a river slowly clogged by debris, leading to a flood upstream. This blockage process is scientifically known as atherosclerosis, a condition that can have significant implications for our heart health. Let’s delve into this complex mechanism to understand what really happens when arteries become blocked and explore the symptoms of blocked arteries in the heart.
Atherosclerosis is a gradual process where the inner walls of the arteries become thickened and narrowed due to the accumulation of plaques. These plaques are made up of fat, cholesterol, calcium, and other substances found in the blood. Think of it as a slow-forming dam inside your arteries, obstructing the smooth flow of blood. This narrowing limits the amount of oxygen-rich blood that can reach vital organs, particularly the heart.
Now, you might be wondering, “How does this process start?” It often begins with damage to the endothelium, the delicate lining of the arteries. Factors such as smoking, high cholesterol, high blood pressure, and diabetes can contribute to this damage. Once the endothelium is compromised, bad cholesterol or LDL (low-density lipoprotein) infiltrates the artery wall and starts to accumulate. The body, in an attempt to heal itself, sends white blood cells to the site, which unfortunately contributes to plaque formation over time.
As the plaque builds up, it can lead to a condition called coronary artery disease (CAD), where the coronary arteries supplying blood to the heart muscle are affected. The symptoms of blocked arteries in the heart can be insidious. Often, people may experience chest pain or discomfort, known as angina, especially during physical exertion. Some might notice shortness of breath or even fatigue, as the heart struggles to get enough oxygen. In severe cases, the plaque can rupture, leading to the formation of a blood clot, which might cause a heart attack.
Understanding these symptoms is crucial for early detection and management. The key takeaway here is that while atherosclerosis develops over time, its effects can be sudden and life-threatening. It’s essential to recognize that the process of artery blockage isn’t just a matter of aging; it’s a complex interplay of lifestyle, genetics, and environmental factors.
In essence, the more we understand about atherosclerosis, the better equipped we are to take proactive steps in maintaining heart health. Regular check-ups and being attentive to any unusual symptoms are vital. Remember, knowledge is power, and understanding what’s happening within your arteries can be the first step towards preventing serious heart conditions.
Reference: National Heart, Lung, and Blood Institute (NHLBI) – “Atherosclerosis” (2023)
The Role of Early Detection in Preventing Atherosclerosis
Importance of Regular Health Screenings in Detecting Early Signs of Atherosclerosis
Imagine trying to stop a train before it gains too much momentum. That’s what early detection aims to do when it comes to atherosclerosis. By catching the signs of blocked arteries in the heart early, we can prevent more severe complications down the line. But how can we identify a problem that often lurks silently within?
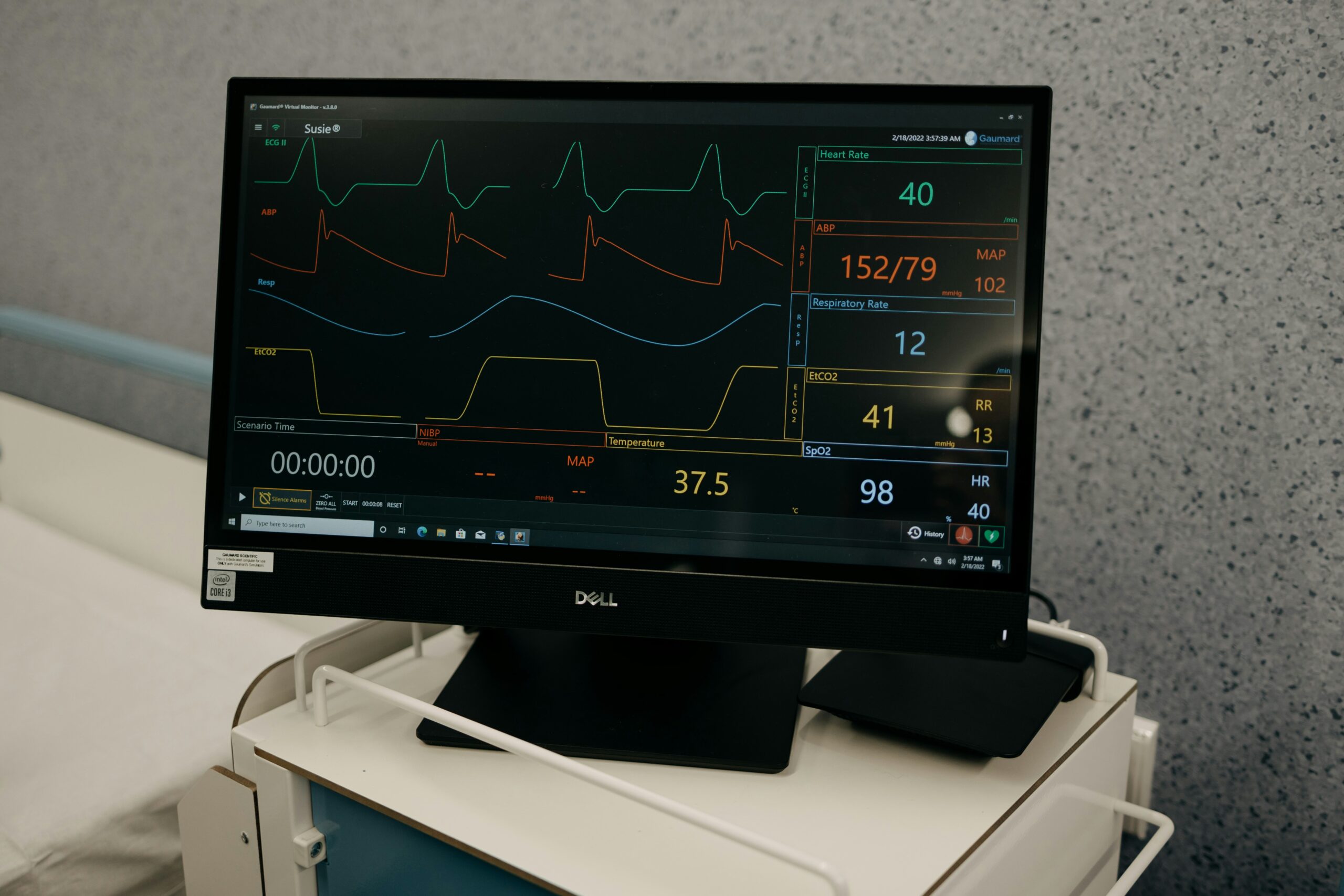
Regular health screenings are like routine maintenance checks for our body. They’re crucial in detecting the early signs of atherosclerosis before they manifest as more pronounced symptoms of blocked arteries in the heart. These screenings can include blood tests to check cholesterol levels, blood pressure measurements, and specialized imaging tests like an electrocardiogram (ECG) or a stress test. These assessments offer a window into the health of our cardiovascular system.
One might ask, “Why should I be concerned about these screenings if I feel perfectly fine?” It’s a valid question. The insidious nature of atherosclerosis means it often progresses quietly, without obvious symptoms until a significant blockage occurs. By then, the risk of heart attack or stroke becomes more imminent. Regular screenings can pick up on the subtle signs that might otherwise go unnoticed, such as elevated cholesterol or high blood pressure, both key contributors to artery blockage.
Consider the analogy of a car engine: it might run smoothly on the surface, but if the oil is low or the engine parts are wearing out, ignoring these issues could lead to a breakdown. Similarly, our bodies might seem to function well, yet underlying issues can be quietly accumulating. Through consistent monitoring, healthcare professionals can identify these early warning signs and suggest interventions to halt or even reverse the progression.
Moreover, early detection provides an opportunity to implement lifestyle changes and medical interventions that can significantly alter the course of the disease. Whether it’s adopting a heart-healthy diet, increasing physical activity, or starting medication, these steps are more effective when initiated early. The knowledge gained from regular health screenings empowers individuals to make informed decisions about their health.
In summary, the role of early detection in preventing atherosclerosis cannot be overstated. By identifying the early signs of blocked arteries in the heart, we can take proactive measures to protect our cardiovascular health. Remember, prevention is not just better than cure—it’s often simpler, less invasive, and a lot less stressful. So, let’s embrace regular health screenings as an integral part of our wellness journey. After all, keeping a close eye on our heart health today can save us from significant heartache tomorrow.
Reference: American Heart Association (AHA) – “Understanding the Importance of Heart Health Screenings” (2023)
An In-Depth Look at Coronary Artery Disease and Its Impact
Understanding the Pathophysiology of Coronary Artery Disease and its Effects on the Heart
Coronary Artery Disease (CAD) is often referred to as the silent saboteur of heart health. At its core, CAD is the result of atherosclerosis affecting the coronary arteries, those tiny vessels responsible for delivering oxygen-rich blood to the heart muscle. But how exactly does it impact the heart, and why should we be concerned about the symptoms of blocked arteries in the heart?
The pathophysiology of CAD begins with the same process of plaque accumulation that characterizes atherosclerosis. As these plaques grow, the lumen, or the inner space of the coronary arteries, becomes progressively narrower. This narrowing impedes blood flow, similar to how a kink in a garden hose restricts water flow. The heart muscle, deprived of adequate oxygen and nutrients, struggles to perform efficiently, especially during physical exertion or stress when the demand for oxygen is higher.
This restricted blood flow manifests as angina, or chest pain, one of the most common symptoms of blocked arteries in the heart. The pain often feels like pressure or squeezing in the chest, sometimes radiating to the shoulders, neck, or arms. It’s a stark reminder that the heart is not receiving enough oxygen. Other symptoms might include shortness of breath, dizziness, or even heart palpitations, which can be alarming signals that the heart is under duress.
When the plaque within the coronary arteries becomes unstable and ruptures, it can lead to the formation of a blood clot. This clot can abruptly block the artery, completely cutting off blood supply to part of the heart muscle. This is what we commonly know as a heart attack, a medical emergency that requires immediate intervention to prevent significant heart damage or death.
The impact of CAD extends beyond the immediate symptoms. Over time, the reduced blood flow can weaken the heart muscle, leading to heart failure, where the heart cannot pump blood effectively to meet the body’s needs. It also increases the risk of arrhythmias, which are irregular heartbeats that can be life-threatening.
Understanding the pathophysiology of CAD underscores the importance of recognizing the symptoms of blocked arteries in the heart. Early intervention can prevent the progression of CAD and mitigate its severe consequences. Lifestyle modifications such as adopting a balanced diet, exercising regularly, and quitting smoking, combined with appropriate medical treatment, can help manage CAD and improve quality of life.
In essence, knowledge about CAD empowers us to take control of our heart health. By being vigilant about symptoms and seeking timely medical advice, we can significantly reduce the burden of this pervasive disease. Remember, our heart is at the center of all that we do—keeping it healthy should be a priority.
Reference: Mayo Clinic – “Coronary Artery Disease: Causes, Symptoms, and Treatment” (2023)
Addressing Common Misconceptions About Atherosclerosis and Aging
Exploring the Relationship Between Aging and Atherosclerosis Development
When it comes to heart health, one persistent myth is that atherosclerosis, or the blockage of arteries, is an inevitable part of aging. While it’s true that the risk increases with age, atherosclerosis is not an unavoidable consequence of getting older. Let’s unpack this relationship and dispel some common misconceptions about how age impacts the symptoms of blocked arteries in the heart.
Firstly, it’s important to understand that atherosclerosis is not a natural part of aging, but rather a disease that can be influenced by various lifestyle and genetic factors. While age does play a role—older individuals are more likely to experience symptoms of blocked arteries in the heart due to longer exposure to risk factors—it’s not the sole determinant. In other words, age alone does not seal your fate when it comes to heart disease. Learn more about aging of the heart in our article
One common misconception is that because atherosclerosis often develops over decades, its symptoms, such as chest pain or shortness of breath, are just a normal part of aging. However, these symptoms are not merely signs of getting older; they are indicators that the heart is struggling to function due to restricted blood flow. It’s crucial for people to recognize that these symptoms warrant medical attention, regardless of age.
Furthermore, many believe that once you reach a certain age, lifestyle changes won’t make a difference in preventing or managing atherosclerosis. This couldn’t be further from the truth. In fact, research shows that adopting a heart-healthy lifestyle can significantly reduce the risk of developing symptoms of blocked arteries in the heart, even later in life. This includes maintaining a balanced diet, engaging in regular physical activity, and managing stress.
It’s also worth noting that while genetics can predispose individuals to atherosclerosis, lifestyle choices have a profound impact on how these genetic factors manifest. This means that even if heart disease runs in your family, you have the power to influence your heart health through proactive measures.
In summary, while aging is a risk factor for atherosclerosis, it is not an inescapable fate. By understanding the distinction between age-related changes and the pathological process of artery blockage, we can take meaningful steps to protect our heart health at any age. Remember, it’s never too late to make changes that can enhance your quality of life and reduce the burden of heart disease. Let’s embrace a proactive approach to aging, where heart health remains a priority throughout all stages of life.
Reference: American College of Cardiology (ACC) – “Aging and Heart Disease: Myth versus Reality” (2023)
Effective Treatments for Managing Atherosclerosis and Heart Health
A Multifaceted Approach: Combining Medication and Lifestyle Changes for Atherosclerosis Management
When it comes to managing atherosclerosis, addressing the symptoms of blocked arteries in the heart requires a comprehensive strategy that combines both medical intervention and lifestyle changes. It’s not about choosing one over the other, but rather integrating these approaches to optimize heart health and prevent further complications.
The cornerstone of medical treatment for atherosclerosis often involves medications that help manage risk factors and symptoms. For instance, statins are commonly prescribed to lower cholesterol levels, a key contributor to plaque formation. By reducing the amount of LDL (bad) cholesterol in the blood, statins can slow the progression of atherosclerosis and decrease the likelihood of developing severe symptoms like chest pain or even a heart attack.
In addition to statins, other medications such as antihypertensives can help control blood pressure, another significant risk factor for blocked arteries. For those who already experience symptoms of blocked arteries in the heart, medications like beta-blockers may be used to reduce heart workload and alleviate angina.
However, medication is just one piece of the puzzle. Lifestyle modifications play an equally vital role in managing atherosclerosis and improving overall heart health. A heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can help maintain optimal cholesterol levels and support cardiovascular health. Moreover, reducing salt intake can assist in managing blood pressure, further protecting the arteries.
Regular physical activity is another crucial component. Engaging in moderate exercise, such as brisk walking, swimming, or cycling, can strengthen the heart muscle, improve circulation, and help maintain a healthy weight. Exercise also has the added benefit of reducing stress, which can have a positive impact on heart health.
Smoking cessation is perhaps one of the most impactful changes one can make. Smoking damages the arteries and accelerates the atherosclerotic process, significantly increasing the risk of heart disease. By quitting smoking, individuals can dramatically reduce their risk and improve their overall health.
It’s also important to manage stress through techniques like mindfulness, yoga, or meditation, as chronic stress can contribute to heart disease. A holistic approach that includes both physical and mental well-being is essential for managing atherosclerosis effectively.
In conclusion, managing atherosclerosis and the symptoms of blocked arteries in the heart requires a multifaceted approach. By combining medication with lifestyle changes, individuals can take control of their heart health and reduce the risk of serious complications. Remember, an integrated strategy is not just about preventing disease, but about enhancing quality of life and longevity. Together, we can take proactive steps towards a healthier heart.