Exploring the Intricacies of Myocarditis: A Comprehensive Overview
Understanding the Intricate Web of Causes Behind Myocarditis: Viral, Bacterial, and Fungal Origins
Picture this: your heart, a tireless organ tirelessly pumping life through your veins, suddenly finds itself under siege. The culprits? Often, they are invisible invaders like viruses, bacteria, and fungi. Myocarditis, a condition characterized by inflammation of the heart muscle, is a complex tapestry woven from these microbial threads. But what exactly triggers this inflamed heart symptoms, and why does it matter?
Let’s start with viruses, the most common instigators of myocarditis. Picture them as tiny hijackers, slipping into your cells and turning them into viral factories. Common viruses such as the Coxsackie B virus, adenoviruses, and even the humble influenza virus can be behind the scenes of myocarditis. In some cases, the inflammation they cause can be severe enough to disrupt the heart’s ability to pump effectively, leading to inflamed heart symptoms like shortness of breath, fatigue, and chest pain.
Now, onto bacteria. Though less common, bacterial infections can also lead to myocarditis. Think of bacteria like group A Streptococcus, known for causing throat infections, which can sometimes lead to a serious complication called rheumatic fever. This condition is akin to a misguided immune response where your body, in an attempt to fend off the bacterial invaders, inadvertently attacks its own heart tissue.
Fungi, the least common of the trio, are like the rare guests at a party you didn’t quite expect. Fungal myocarditis is typically seen in individuals with weakened immune systems, where fungi like Candida or Aspergillus seize the opportunity to invade. Their presence can lead to inflamed heart symptoms that mimic those caused by their viral and bacterial counterparts.
But why does this all matter? Understanding the root causes of myocarditis is crucial because it informs how we approach treatment. For instance, antiviral medications may be considered when a viral infection is suspected, while antibiotics are the go-to for bacterial infections. Fungal infections, on the other hand, require antifungal agents.
In summary, the intricate causes of myocarditis—whether viral, bacterial, or fungal—underscore the importance of recognizing inflamed heart symptoms early. The earlier we identify the culprit, the sooner we can tailor the right response, safeguarding the heart’s precious rhythm. The key takeaway? Always tune in to your body’s signals and seek medical advice if those heart symptoms arise. Your heart, after all, deserves the best defense we can muster.
Reference: Caforio AL, Pankuweit S, Arbustini E, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. European Heart Journal. 2013;34(33):2636-2648.
Understanding the Link Between Myocarditis and Pericarditis
Differentiating Between Myocarditis and Pericarditis: Causes, Symptoms, and Diagnostic Criteria
Imagine your heart as a house. The walls of this house are the heart muscle—this is where myocarditis resides. The pericardium, on the other hand, is like the fence surrounding the house, a protective layer that keeps things in order. When we talk about myocarditis and pericarditis, we are essentially discussing inflammation of these two different, yet closely related, parts of the heart. So, how do we differentiate between these two conditions, especially when they both can stir up a storm of inflamed heart symptoms?
Let’s start with myocarditis. As we explored in the previous section, myocarditis involves inflammation of the heart muscle itself. The usual suspects include viral infections, but autoimmune diseases and drug reactions can also play a role. Symptoms can range from being subtle, like fatigue and mild chest discomfort, to more severe manifestations such as heart palpitations and shortness of breath.
Now, shifting our focus to pericarditis, this condition affects the pericardium, the sac-like structure enveloping your heart. Imagine it as the heart’s personal security detail, and it’s under threat. Viral infections are again often to blame, but other causes like autoimmune conditions (think lupus) or even a heart attack can trigger pericarditis. Common symptoms include sharp chest pain that often worsens with deep breaths or when lying flat—a hallmark differentiator from myocarditis.
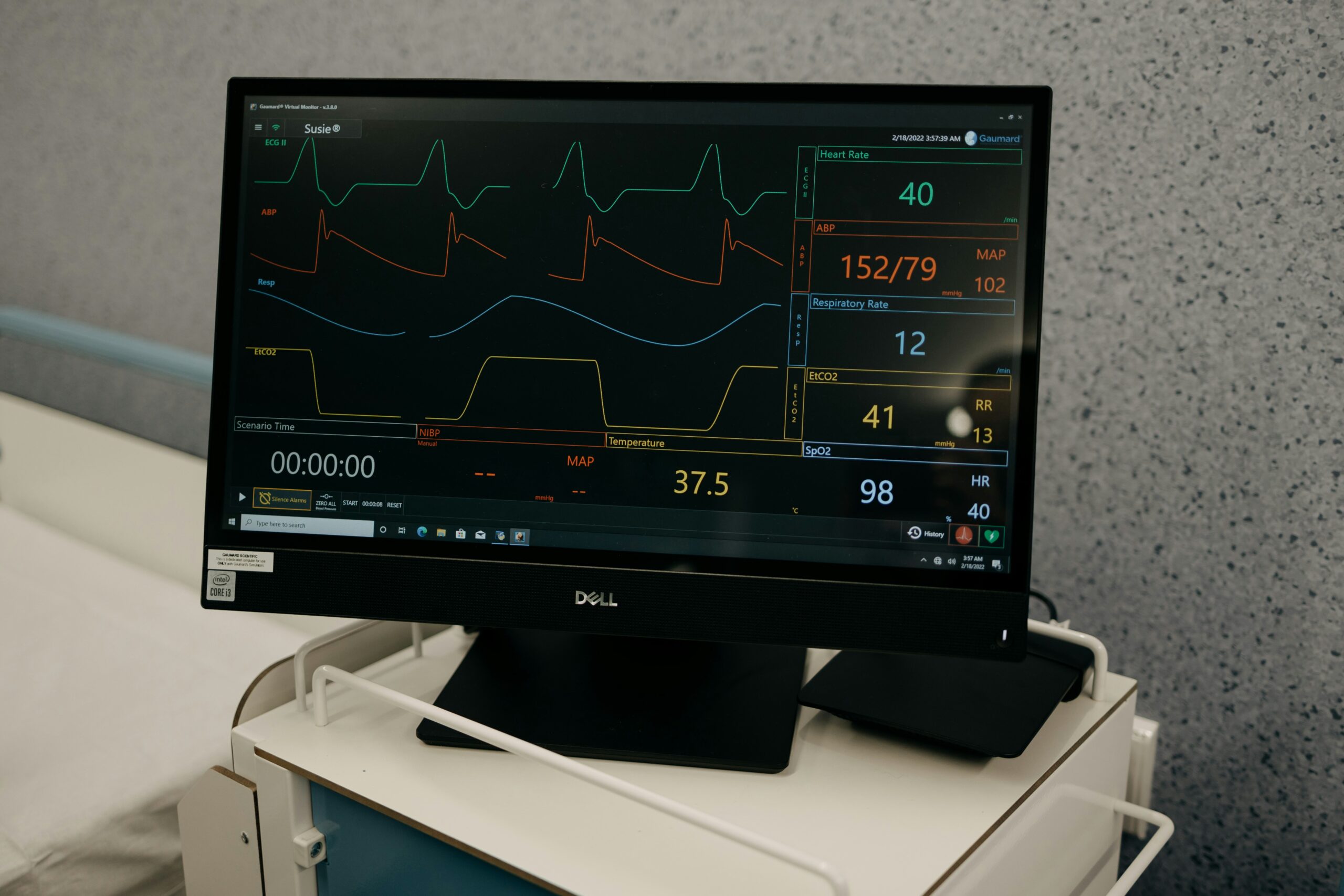
Diagnosing these conditions involves a blend of detective work and modern medicine. An electrocardiogram (ECG) can reveal distinct patterns for each condition. In pericarditis, you might find a signature ST elevation across several leads, while myocarditis can result in non-specific changes or even mimic a heart attack. Imaging studies like echocardiograms can provide a visual confirmation, showing any inflammation or fluid accumulation around the heart.
Blood tests also play a pivotal role. Cardiac biomarkers, for instance, can indicate heart muscle damage in myocarditis, while inflammatory markers might be elevated in both conditions. Additionally, a definitive diagnosis might sometimes require a heart MRI or even a biopsy to pinpoint the exact nature of the inflammation.
Understanding these distinctions is crucial for treatment. While both conditions may require anti-inflammatory medications, specific therapies can vary. Myocarditis might necessitate antivirals or immunosuppressive drugs, while pericarditis might respond well to colchicine or corticosteroids.
In essence, while myocarditis and pericarditis share the spotlight in the realm of inflamed heart symptoms, recognizing their unique traits helps us tailor the right approach to safeguarding our heart’s health. By knowing the difference, we empower ourselves to seek timely medical intervention, ensuring that our heart, both the house and its fence, remains protected and resilient.
Reference: Imazio M, Adler Y. Management of Pericardial Effusion. European Heart Journal. 2013;34(16):1186-1197.
Differentiating Acute and Chronic Myocarditis: What You Need to Know
Distinguishing Between Acute and Chronic Myocarditis: Understanding the Timeline and Progression of Each Condition
Imagine you’re on a journey, and suddenly, you encounter two paths. One is a short, intense burst of activity, while the other stretches out into a long, winding road with persistent challenges. This analogy mirrors the difference between acute and chronic myocarditis. Both involve the inflamed heart, yet they unfold in remarkably different ways, each with its own set of symptoms and implications.
Acute myocarditis is like a sudden storm. It strikes quickly, often with little warning. The inflamed heart symptoms can be dramatic: sudden chest pain, fatigue, shortness of breath, and even palpitations. This form of myocarditis is usually tied to a recent viral infection, and the immune system’s response can be intense, leading to significant inflammation of the heart muscle. The good news? Acute myocarditis often improves with rest and treatment, and many people recover fully.
Chronic myocarditis, on the other hand, is akin to a persistent drizzle that just won’t quit. It develops slowly and can last for months or even years. Here, the symptoms might be less dramatic, often manifesting as lingering fatigue, mild chest discomfort, or a subtle decline in exercise tolerance. The causes of chronic myocarditis can be multifaceted, ranging from ongoing autoimmune processes to prolonged exposure to toxins or infections. This sustained inflammation can lead to more serious complications over time, such as heart failure.
Diagnosing the type of myocarditis involves a combination of clinical evaluation, imaging, and sometimes tissue biopsy. In acute cases, doctors often rely on blood tests to detect markers of heart injury and inflammation, coupled with imaging techniques like echocardiograms or MRIs to visualize the heart’s condition. Chronic myocarditis might require more in-depth investigation to uncover underlying causes, and repeated imaging may be used to monitor progression over time.
Understanding the distinction between acute and chronic myocarditis is crucial for crafting an effective treatment plan. Acute cases might respond well to supportive care and anti-inflammatory medications, whereas chronic myocarditis may necessitate more targeted therapies, including immunosuppressants or lifestyle adjustments to manage long-term heart health.
Ultimately, whether facing the sudden storm of acute myocarditis or navigating the long road of chronic myocarditis, recognizing the symptoms and seeking timely medical care is key. By distinguishing between these two paths, we can better equip ourselves to manage the journey and protect our heart’s vitality for the long haul.
Reference: Cooper LT. Myocarditis. New England Journal of Medicine. 2009;360(15):1526-1538.
Recognizing the Symptoms of Myocarditis: A Vital Checklist
Highlighting Key Red Flags on the Myocarditis Symptom Checklist That Warrant Immediate Medical Attention
Imagine your heart sending out distress signals, much like a ship in turbulent seas. Recognizing these signals, especially when it comes to myocarditis, is crucial. When it comes to inflamed heart symptoms, knowing what to look for can make all the difference in seeking timely medical intervention.
First on the checklist is chest pain. This isn’t your typical muscular ache post-gym session. Instead, think sharp, stabbing sensations or a persistent discomfort that refuses to fade. It’s the kind of pain that makes you sit up and take notice, often accompanied by a feeling of tightness or pressure.
Next, we have shortness of breath. This can feel like you’ve just sprinted a marathon, even if you’ve only climbed a flight of stairs. Your heart, struggling with inflammation, may not pump as efficiently, leading to this breathlessness—especially noticeable during physical activity or even at rest.
Fatigue is another telltale symptom. It’s not just the result of a late night or a busy week. This is an overwhelming exhaustion that leaves you drained, affecting your daily life and activities. It’s as if your body is constantly running on empty, despite adequate rest.
Palpitations also make the list. Imagine your heart performing an erratic dance, skipping beats or pounding unusually hard. These irregular heartbeats can be disconcerting, often causing anxiety and a sense of unease.
Fever and flu-like symptoms can also accompany myocarditis, especially if a viral infection is at play. These symptoms might seem ordinary, but when combined with the aforementioned heart-related symptoms, they become more significant.
In some cases, you might also experience swelling in your legs or abdomen, known as edema. This occurs when the heart’s function is compromised, leading to fluid retention—a clear signal that warrants attention.
It’s important to remember that these symptoms can vary in intensity and presentation. Some individuals might experience all of them, while others might notice only a few. However, the presence of these symptoms, particularly if they manifest suddenly or intensify quickly, should prompt immediate medical evaluation.
Understanding and recognizing this checklist of inflamed heart symptoms empowers you to act swiftly. If you or someone you know experiences these symptoms, seeking medical advice is crucial. Early detection and intervention can significantly impact the course of myocarditis, helping to protect your heart from further damage and ensuring it remains robust and resilient.
Reference: Kindermann I, Barth C, Mahfoud F, et al. Update on Myocarditis. Journal of the American College of Cardiology. 2012;59(9):779-792.
Preventing Myocarditis: Strategies to Safeguard Your Heart Health
Exploring Lifestyle Modifications, Including a Heart-Healthy Diet and Regular Exercise, as Key Preventive Measures Against Myocarditis
Imagine your heart as a loyal teammate, working tirelessly to keep you in the game of life. To ensure it’s in peak condition and resilient against conditions like myocarditis, incorporating preventive strategies is key. While we can’t control every factor, such as genetic predispositions, we can certainly influence lifestyle choices that bolster heart health and minimize the risk of inflamed heart symptoms.
First and foremost, let’s talk about diet. Picture your plate as a palette, filled with vibrant colors and wholesome, nutrient-rich foods. A heart-healthy diet emphasizes fruits, vegetables, whole grains, lean protein sources, and healthy fats—think olive oil, nuts, and avocados. Learn more about healthy eating in our article. These foods are packed with antioxidants, vitamins, and minerals that support cardiovascular health. Reducing intake of processed foods, sugars, and saturated fats is equally important, as these can contribute to inflammation and heart strain.
Regular exercise is another cornerstone of heart health. Imagine your heart as a muscle that thrives on movement. Engaging in regular physical activity strengthens the heart, improves circulation, and helps maintain a healthy weight—all factors that reduce the risk of myocarditis. Aim for at least 150 minutes of moderate aerobic exercise, such as brisk walking or cycling, each week. Incorporating strength training exercises twice a week also provides added benefits.
Managing stress is another crucial strategy. Chronic stress can lead to increased inflammation in the body, potentially impacting heart health. Techniques such as mindfulness, meditation, yoga, or even simple deep-breathing exercises can be powerful tools in reducing stress levels. Think of these practices as a mental reset, calming the mind and, by extension, the heart.
Avoiding infections is particularly relevant when it comes to preventing myocarditis, which often follows viral illnesses. Simple measures such as regular handwashing, staying up-to-date with vaccinations, and avoiding close contact with individuals who are ill can reduce your risk of infections that might lead to heart inflammation.
Lastly, regular medical check-ups play a vital role in prevention. These visits offer an opportunity to monitor heart health indicators, address concerns, and make informed decisions about lifestyle and medical interventions if necessary.
By embracing these lifestyle modifications, we create a protective shield around our hearts, minimizing the risk of myocarditis and its inflamed heart symptoms. The journey to heart health is ongoing, but with each step, we fortify our hearts against potential challenges, ensuring they continue to beat strong and steady through the many seasons of life.
Reference: Glezeva N, Baugh J. Myocarditis: current trends in diagnosis and treatment. Trends in Cardiovascular Medicine. 2014;24(6):273-281.