Understanding the Progression: What is Stage 5 Congestive Heart Failure?
Defining Stage 5 CHF: The Final Stage of a Progressive Condition
Imagine a journey that starts with a gentle uphill walk and gradually becomes a steep and challenging climb. This metaphor aptly describes the progression of congestive heart failure (CHF). At Stage 5, we’ve reached the summit, where the climb is steepest and every step requires significant effort. Stage 5 congestive heart failure represents the final stage, often referred to as end-stage CHF, where the heart’s ability to pump blood has severely declined, and symptoms are persistent despite treatment. Mayo Clinic – Heart failure
In simpler terms, think of your heart as a pump. In the earlier stages of CHF, this pump might be working a bit harder to keep up with demands. By the time we reach stage 5, the pump is struggling to function effectively, leading to a cascade of symptoms that impact daily life. These symptoms can include severe fatigue, difficulty breathing, and swelling in the legs and abdomen.
The Journey to Stage 5: A Progressive Condition
To truly grasp Stage 5 CHF, it’s important to understand the path leading up to it. Congestive heart failure doesn’t happen overnight. It’s a chronic condition that typically progresses through stages, often starting with subtle signs that are easy to overlook. Early stages might involve minor symptoms like shortness of breath during physical activities or slight swelling in the ankles, which can be mistaken for signs of aging or being out of shape.
As CHF progresses, the symptoms become more pronounced and frequent, signaling that the heart’s efficiency is declining. By Stage 5, the heart’s capacity to circulate blood is severely compromised, affecting multiple organs and systems within the body. This stage is characterized by frequent hospitalizations and a significant decline in the ability to perform daily activities. Patients may find themselves needing more frequent medical interventions and support to manage symptoms.
Living with Stage 5 CHF: The Human Experience
Living with stage 5 congestive heart failure is akin to navigating a complex maze. Every turn presents a new challenge, and the way forward isn’t always clear. For patients, this stage demands not just medical care, but emotional and psychological support. It’s a time when patients and their families often have to make difficult decisions about treatment options and quality of life, emphasizing the need for comprehensive care approaches.
The reality of Stage 5 CHF is daunting, but it also underscores the importance of early detection and management of heart failure. By understanding the signs and progression of CHF, individuals can seek medical advice sooner, potentially slowing the progression and improving quality of life.
In summary, Stage 5 congestive heart failure marks the final and most severe stage of this chronic condition. It is a time when the heart’s ability to function is significantly impaired, leading to a range of complex symptoms that require careful management and support. Understanding this stage is crucial for patients, caregivers, and healthcare providers alike, as it shapes the approach to care and decision-making.
Reference:
- Ponikowski, P., Voors, A. A., Anker, S. D., Bueno, H., Cleland, J. G. F., Coats, A. J. S., … & van der Meer, P. (2016). 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). European Heart Journal, 37(27), 2129-2200.
Exploring the Link: High Heart Rate and Palpitations in Stage 5 CHF
Understanding the Impact: How High Heart Rate Affects Stage 5 CHF Patients
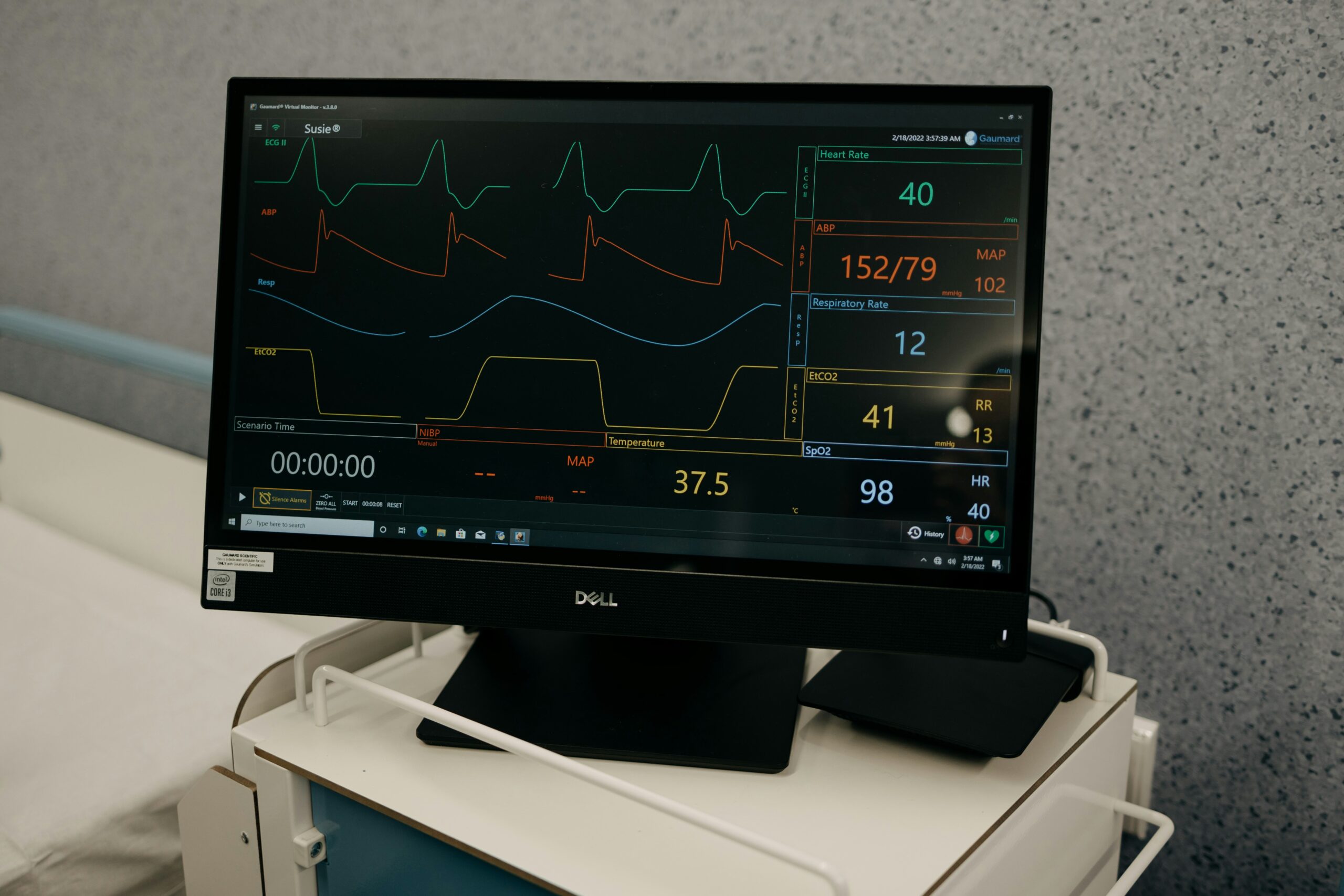
Picture your heart as an engine. In stage 5 congestive heart failure, this engine is working overtime, often resulting in an elevated heart rate or palpitations. These symptoms are not just inconvenient; they are significant indicators of how hard the heart is working to compensate for its diminished function.
In stage 5 CHF, the heart is under tremendous strain. It’s as if the engine is being revved up constantly, trying to maintain speed despite having less power. A high heart rate in this context is the heart’s attempt to pump more blood to meet the body’s demands. Unfortunately, this is not a sustainable solution. Over time, the increased heart rate can lead to further deterioration of heart muscle function and exacerbate symptoms. National Library of Medicine – Tachycardia in Heart Failure
The Role of Palpitations: More Than Just a Flutter
Palpitations, those rapid or irregular heartbeats that can feel like a fluttering or pounding in the chest, are common in patients with stage 5 congestive heart failure. While they may occur sporadically in healthy individuals, in the context of CHF, they signal an underlying issue with the heart’s electrical system. This can lead to arrhythmias, which are abnormal heart rhythms that further impair the heart’s ability to pump effectively.
Imagine trying to run a marathon while someone is constantly tapping you on the shoulder. This is akin to how palpitations can distract and disrupt the heart’s function in CHF patients. For individuals with advanced heart failure, these palpitations can be distressing, contributing to increased anxiety and a sense of being unwell.
Managing High Heart Rate and Palpitations in Stage 5 CHF
Addressing high heart rate and palpitations in stage 5 CHF involves a multifaceted approach. Medications such as beta-blockers may be prescribed to help control the heart rate and reduce the frequency of palpitations. These medications work by slowing down the heart, allowing it to pump more efficiently without overexerting itself.
In addition to medication, lifestyle modifications can also play a crucial role. Patients are often advised to avoid stimulants like caffeine and nicotine, which can exacerbate palpitations and increase heart rate. Stress management techniques, such as mindfulness and relaxation exercises, can also be beneficial in reducing the impact of these symptoms.
The Bigger Picture: Why Monitoring Matters
Monitoring heart rate and palpitations in stage 5 congestive heart failure is critical. These symptoms provide valuable insights into the heart’s current state and can guide treatment decisions. Regular check-ups and communication with healthcare providers are essential for managing these symptoms effectively and improving overall quality of life.
In conclusion, a high heart rate and palpitations are more than just symptoms in stage 5 congestive heart failure; they are indicators of the heart’s struggle to cope with its declining function. Understanding and managing these symptoms is a vital part of care, helping patients navigate their condition with greater awareness and support.
Reference:
- Yancy, C. W., Jessup, M., Bozkurt, B., Butler, J., Casey Jr, D. E., Drazner, M. H., … & Wilkoff, B. L. (2013). 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation, 128(16), 1810-1852.
Edema and Fluid Build-Up: A Common Symptom of End-Stage CHF
Complications and Consequences: Exploring the Risks Associated with Edema in CHF
Consider a sponge that has been saturated with water. No matter how much you try to wring it out, the water keeps seeping back in. This is what happens in stage 5 congestive heart failure when it comes to fluid retention and edema. Edema, or swelling caused by fluid build-up, is a hallmark symptom of end-stage CHF, reflecting the heart’s inability to manage the fluid balance efficiently.
At this advanced stage of congestive heart failure, the heart’s compromised function leads to poor circulation. This results in the kidneys receiving less blood flow, which triggers them to retain sodium and water, exacerbating fluid build-up. The excess fluid then accumulates in various parts of the body, often manifesting as swelling in the legs, ankles, and abdomen.
Understanding the Risks: More Than Just Swelling
While edema can seem like a mere inconvenience, in stage 5 CHF, it signifies deeper systemic issues. The pooled fluid can lead to discomfort and mobility challenges, significantly impacting a patient’s quality of life. But the risks run deeper. Fluid retention can strain the heart further, leading to increased pressure in the blood vessels and worsening heart function.
Moreover, fluid build-up in the lungs, known as pulmonary edema, can occur. This condition makes breathing difficult and can be life-threatening if not addressed promptly. Imagine trying to breathe with a heavy weight on your chest; this is how pulmonary edema can feel for those with stage 5 congestive heart failure.
Managing Edema: Strategies for Control
Managing edema in stage 5 CHF requires a comprehensive approach. Diuretics, often referred to as “water pills,” are commonly prescribed to help the body expel excess fluid. These medications prompt the kidneys to release more sodium and water, reducing swelling and easing the burden on the heart.
In addition to medication, dietary adjustments are crucial. Reducing salt intake can help prevent further fluid retention. Patients are often advised to monitor their fluid intake and weight daily to detect any significant changes early. Elevating the legs can also aid in reducing swelling in the lower extremities.
The Importance of Vigilance: Monitoring and Support
Close monitoring and regular communication with healthcare providers are vital in managing edema effectively. Patients with stage 5 congestive heart failure must work closely with their medical team to adjust treatment plans as needed, ensuring that fluid retention is kept in check.
In conclusion, edema and fluid build-up are more than just symptoms in stage 5 congestive heart failure; they are indicators of the heart’s struggle with fluid management. Understanding these symptoms and their implications is essential for effective management, helping to alleviate discomfort and improve the overall quality of life for those affected.
Reference:
- McMurray, J. J., Adamopoulos, S., Anker, S. D., Auricchio, A., Böhm, M., Dickstein, K., … & Zannad, F. (2012). ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. European Heart Journal, 33(14), 1787-1847.
Cognitive Changes and Confusion: How CHF Affects Mental Health
The Mind-Heart Connection: Exploring the Link Between CHF and Cognitive Changes
Imagine trying to solve a complex puzzle when the pieces keep changing shape. This is what cognitive changes can feel like for someone with stage 5 congestive heart failure. At this advanced stage, the heart’s impaired function can lead to reduced blood flow to the brain, resulting in a range of cognitive symptoms, including confusion, memory loss, and difficulties with concentration.
The heart and brain are intricately connected, and when the heart struggles, the brain often feels the impact. In stage 5 CHF, decreased cardiac output means less oxygen and nutrients are delivered to the brain. This can manifest as “brain fog,” where mental clarity is compromised, making everyday tasks seem daunting and complex.
Understanding the Cognitive Impact: More Than Just Forgetfulness
Cognitive changes in stage 5 CHF are not simply about occasional forgetfulness. They can profoundly affect a person’s ability to manage their health and daily life. Imagine trying to remember medication schedules or follow complex medical instructions while feeling mentally overwhelmed. This underscores the importance of recognizing and addressing cognitive symptoms as part of managing end-stage heart failure.
Confusion, a common cognitive change, can be particularly distressing for both patients and their families. It may lead to disorientation, making familiar environments seem unfamiliar. This can increase the risk of accidents and affect a person’s ability to engage in meaningful interactions, further impacting their quality of life.
Addressing Cognitive Symptoms: Strategies for Support
Managing cognitive changes in stage 5 congestive heart failure requires a holistic approach. Healthcare providers often recommend cognitive assessments to identify specific areas of concern. This can help tailor interventions to support mental function, such as cognitive exercises or memory aids.
Additionally, ensuring optimal heart health through medication adherence and lifestyle modifications can indirectly support cognitive health. Adequate management of heart failure symptoms can improve overall circulation, potentially benefiting brain function.
The Role of Emotional Support: Navigating Cognitive Challenges
Living with cognitive changes can be emotionally taxing. Patients may experience frustration or embarrassment over cognitive lapses, leading to increased anxiety or depression. Emotional support, whether through counseling or support groups, can play a crucial role in helping individuals navigate these challenges.
Family members and caregivers also play an essential role in providing support. They can help with organizing daily routines, managing medications, and offering reassurance during moments of confusion. By fostering a supportive environment, patients with stage 5 congestive heart failure can better cope with cognitive changes.
In summary, the cognitive changes associated with stage 5 congestive heart failure highlight the profound connection between heart and brain health. Recognizing and addressing these changes is vital for comprehensive care, ensuring that patients receive the support they need to maintain mental clarity and enhance their quality of life.
Reference:
- Hajduk, A. M., & Krumholz, H. M. (2015). Cognitive impairment in heart failure: a review of the literature (2015). European Journal of Heart Failure, 17(6), 674-682.
Palliative Care: Enhancing Quality of Life in Stage 5 CHF
Symptom Management: Addressing Pain and Discomfort Through Palliative Care in Stage 5 CHF
Imagine you’re navigating through a storm, seeking shelter and relief from the relentless weather. For patients with stage 5 congestive heart failure, palliative care serves as a sanctuary amidst the challenges of their condition. At this advanced stage, where the heart’s functionality is severely compromised, palliative care focuses on improving quality of life by managing symptoms and providing comprehensive support.
Palliative care is not about giving up; it’s about prioritizing comfort and dignity. For individuals with stage 5 CHF, this means addressing both physical symptoms and emotional well-being. Symptom management is a cornerstone of palliative care, helping patients find relief from the persistent discomforts of heart failure, such as pain, shortness of breath, and fatigue.
Tailoring Care: A Personalized Approach to Comfort
One of the most significant aspects of palliative care in stage 5 congestive heart failure is its personalized approach. Care plans are tailored to meet the unique needs and preferences of each patient, ensuring that their specific symptoms are addressed. This might involve adjusting medications to better manage pain and breathlessness or implementing non-pharmacological interventions such as oxygen therapy or relaxation techniques.
Additionally, palliative care teams often include a diverse range of specialists, from doctors and nurses to social workers and spiritual advisors. This multidisciplinary approach ensures comprehensive support, addressing not only physical symptoms but also emotional, social, and spiritual needs.
Emotional and Psychological Support: Navigating the Journey
Living with stage 5 congestive heart failure can be emotionally overwhelming. Patients may experience feelings of anxiety, depression, or fear about the future. Palliative care provides crucial emotional and psychological support, offering counseling and therapeutic interventions to help patients and their families cope with these challenges.
Support groups can also be an invaluable resource, providing a sense of community and understanding. Sharing experiences with others who are navigating similar journeys can offer comfort and reduce the sense of isolation that often accompanies chronic illness.
Planning for the Future: Empowering Patients and Families
Palliative care in stage 5 CHF also involves planning for the future. This includes discussions about advanced care planning and end-of-life preferences, empowering patients to make informed decisions about their care. These conversations, though difficult, are essential in ensuring that patients’ wishes are respected and that they receive the care they desire.
In conclusion, palliative care plays a vital role in enhancing the quality of life for patients with stage 5 congestive heart failure. By focusing on symptom management, emotional support, and future planning, palliative care offers a compassionate approach to care, helping patients navigate their journey with dignity and comfort.
Learn more about heart and vascular disease in our article on atherosclerosis
Reference:
- Bekelman, D. B., Havranek, E. P., Becker, D. M., Kutner, J. S., Peterson, P. N., Wittstein, I. S., & Gottlieb, S. H. (2007). Symptoms, depression, and quality of life in patients with heart failure. Journal of Cardiac Failure, 13(8), 643-648.