Arrhythmia and Atrial Fibrillation: A Comprehensive Guide
Understanding the Fundamental Differences Between Arrhythmia and Atrial Fibrillation
Let’s embark on a journey through the heart’s complex landscape, where the terms “arrhythmia” and “atrial fibrillation” often pop up. To those unacquainted, they might sound like interchangeable jargon, but they mark distinct territories in the realm of cardiac health. So, what sets them apart, and why should we care?
Arrhythmia, in its broadest sense, refers to any irregularity in the heart’s rhythm. Imagine the heart as a meticulous orchestra, where every beat is a note played with precision. When arrhythmia strikes, it’s like a musician playing out of sync; sometimes, the heart beats too fast (tachycardia), too slow (bradycardia), or irregularly. Arrhythmia can range from benign hiccups in the heart’s rhythm to more sinister patterns that signal underlying cardiac issues.
Enter atrial fibrillation, or AFib, a specific type of arrhythmia that deserves its spotlight. In atrial fibrillation, the heart’s upper chambers (the atria) quiver chaotically, almost as if the musicians in our orchestra decide to play their own tunes. This disarray disrupts the orderly flow of blood and can lead to pooling, increasing the risk of clots. These clots are the stealthy culprits behind strokes, making AFib more than just a heart rhythm issue—it’s a significant health concern.
One might ponder, “Why does this happen?” The heart’s electrical system is the conductor that orchestrates the rhythm. In AFib, these electrical signals go haywire, particularly in the atria, creating a cacophony instead of a symphony. This is where our keyword, “arrhythmia atrial fibrillation,” becomes crucial. Understanding AFib’s role as a form of arrhythmia helps us appreciate the nuances of heart health.
It’s worth noting that while all cases of atrial fibrillation are arrhythmias, not all arrhythmias are atrial fibrillation. Other types include ventricular tachycardia, where the lower chambers of the heart are affected, or premature beats, which are usually harmless but can be unsettling.
Why is delineating these differences important? For one, it guides treatment. Treatments tailored for general arrhythmias might not suffice for AFib, which may require more specialized interventions, such as anticoagulants or rhythm control medications.
In summary, while arrhythmia is the broader category, atrial fibrillation is a specific, more notorious member of this family, with its unique challenges and implications. By understanding these distinctions, we’re better equipped to comprehend the implications for health and treatment. For those navigating heart health, recognizing these nuances is the first step towards informed decisions and effective management.
Reference: American Heart Association. “Types of Arrhythmia.” (2023).
Recognizing the Telltale Signs: Symptoms of Atrial Fibrillation
Identifying the Subtle Signs: How Atrial Fibrillation Symptoms Manifest
When it comes to atrial fibrillation, the symptoms can often play a game of hide and seek. Sometimes overt and loud, other times whispering quietly in the background. But how do we, as vigilant guardians of our own health, recognize these signs before they escalate into something more ominous?
Atrial fibrillation, a specific form of arrhythmia, often announces itself with palpitations. Imagine feeling like your heart is performing an enthusiastic drum solo inside your chest. These palpitations can be fast, irregular, or both, leaving you breathless and sometimes even a bit dizzy. However, they’re not the only players in this symphony of symptoms.
Fatigue, perhaps the most insidious symptom, can creep in, making everyday tasks feel like Herculean feats. It’s as if your energy reserves have been mysteriously drained overnight. This weariness can be easily mistaken for stress or overwork, but when combined with other symptoms, it may hint at atrial fibrillation’s presence.
Shortness of breath can also join the ensemble, even during activities that previously didn’t leave you winded. Imagine climbing a flight of stairs and feeling as though you’ve just run a marathon. This symptom can be particularly concerning if it appears suddenly and without a clear explanation.
Some individuals may experience chest discomfort, which can vary from mild pressure to more intense pain. While this can be alarming, it’s crucial to differentiate it from heart attack symptoms. Nevertheless, any form of chest pain warrants immediate medical attention.
Interestingly, atrial fibrillation can sometimes masquerade with no symptoms at all. Known as “silent AFib,” this variant can quietly increase the risk of stroke without the usual warning signs. Silent AFib can only be detected through routine medical check-ups or specific diagnostic tests, emphasizing the importance of regular heart health assessments.
It’s also worth noting that the frequency and intensity of symptoms can vary. For some, they might be occasional visitors, while others may experience persistent symptoms that significantly impact their quality of life.
So, what should we do if we suspect atrial fibrillation is at play? The first step is to consult with a healthcare professional who can provide a proper diagnosis. They might recommend monitoring your heart’s rhythm over time or performing an electrocardiogram to catch AFib in the act.
In essence, being attuned to your body’s signals is key. Recognizing the symptoms of atrial fibrillation early can lead to timely intervention and can significantly reduce the risk of complications such as stroke. By staying informed and proactive, we can better manage our heart health and maintain the rhythm of our lives.
Reference: National Heart, Lung, and Blood Institute. “Signs, Symptoms, and Complications of Atrial Fibrillation.” (2023).
Delving into the Mechanisms Behind Arrhythmia and Atrial Fibrillation
Exploring the Electrical Pathways: How Arrhythmia and Atrial Fibrillation Disrupt Heart Rhythms
Picture the heart as a finely-tuned electrical circuit, where every beat is a well-timed impulse coursing through the heart’s intricate pathways. However, when arrhythmia, particularly atrial fibrillation, disrupts this harmony, it’s akin to a sudden power surge causing chaos in an electrical grid. But how exactly does this disruption occur?
The heart’s rhythmic contractions are orchestrated by electrical signals that originate from the sinoatrial (SA) node, often dubbed the heart’s natural pacemaker. These signals propagate through the atria, prompting them to contract and push blood into the ventricles. In a healthy heart, this process is orderly and sequential. However, in atrial fibrillation, the signals become erratic, primarily within the atria, leading to that infamous quivering instead of a coordinated contraction.
This disruption is due to multiple, rapid electrical impulses firing simultaneously in the atria, overwhelming the SA node. It’s as if several conductors are attempting to lead the orchestra at once, resulting in a cacophony rather than a symphony. This chaotic firing causes the atria to contract in a disorganized manner, which impairs their ability to efficiently move blood into the ventricles.
The ventricles, in response, receive irregular signals and contract at an abnormal rate. This irregularity is what we identify as an arrhythmia. In the case of atrial fibrillation, the heart rate can become rapid and uneven, which not only affects the heart’s efficiency but also increases the workload on the organ.
But what triggers these erratic electrical impulses? Several factors can contribute, including high blood pressure, heart valve diseases, and hyperthyroidism. Additionally, lifestyle factors like excessive alcohol consumption and stress can also play a role in precipitating these irregular heart rhythms.
Understanding these mechanisms is crucial because it guides the development of targeted treatments. For instance, medications that stabilize the heart’s electrical activity or procedures like cardioversion, which “reset” the heart’s rhythm, are designed based on this knowledge of electrical pathway disruptions.
Moreover, identifying and managing underlying conditions that contribute to the chaotic electrical signals can be pivotal in preventing and controlling atrial fibrillation. This underscores the importance of comprehensive cardiovascular health management.
In conclusion, the heart’s electrical system is a marvel of biological engineering, but it is not immune to disturbances. By exploring and understanding how arrhythmia and atrial fibrillation disrupt this system, we gain valuable insights into maintaining our heart’s rhythm and optimizing our overall health.
Reference: Cleveland Clinic. “How the Heart’s Electrical System Works.” (2023).
Diagnostic Tools and Techniques for Atrial Fibrillation Detection
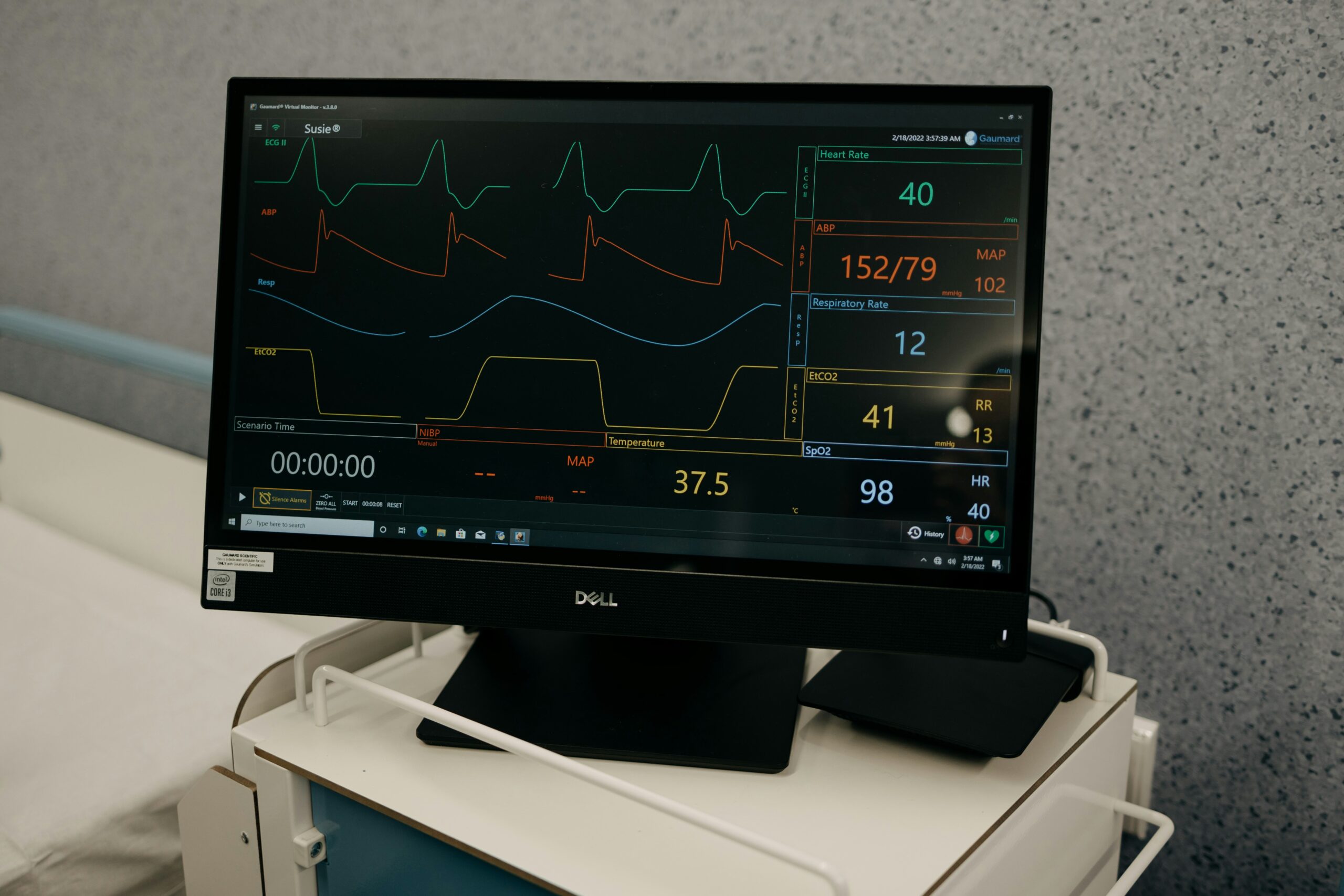
Electrocardiogram (ECG): The Gold Standard for Detecting Atrial Fibrillation
Imagine you’re a detective on a mission to uncover the hidden presence of atrial fibrillation, a common type of arrhythmia. Your most reliable tool in this investigation? The electrocardiogram, or ECG. This non-invasive test is the gold standard for detecting the electrical anomalies characteristic of atrial fibrillation. But how does it work, and what makes it so effective?
An ECG records the electrical activity of the heart through sensors placed on the skin, typically on the chest, arms, and legs. These sensors capture the heart’s electrical signals as they travel through its chambers. The result is a graph—a snapshot of the heart’s rhythm over time. In the case of atrial fibrillation, this graph reveals a telltale pattern: irregular, often rapid heartbeats with no discernible P waves, which represent the atrial contractions in normal sinus rhythm.
Why is the ECG so pivotal in identifying atrial fibrillation? It provides a direct window into the heart’s electrical activity, allowing clinicians to diagnose AFib with precision. This is particularly crucial because atrial fibrillation can sometimes be elusive, especially in cases where symptoms are intermittent or absent.
In addition to standard ECGs, extended monitoring tools like Holter monitors or event recorders can capture arrhythmias over longer periods. These devices are particularly useful for diagnosing paroxysmal atrial fibrillation, where episodes occur sporadically and might be missed during a standard ECG.
Blood Tests: Biomarkers and Lab Values in Atrial Fibrillation Diagnosis
While ECGs are central to identifying arrhythmia atrial fibrillation, blood tests also play a supporting role. They help uncover underlying conditions that might contribute to AFib or assess its impact on the body. For instance, tests measuring thyroid hormone levels can identify hyperthyroidism, a known trigger for atrial fibrillation. Similarly, electrolyte imbalances, which can provoke arrhythmias, are detectable through routine blood work.
Additionally, blood tests can check for biomarkers associated with heart stress or damage, such as B-type natriuretic peptide (BNP) or troponin. Elevated levels might not only indicate atrial fibrillation but also signal potential complications, like heart failure.
Together, ECGs and blood tests form a comprehensive diagnostic approach. They enable healthcare providers to confirm the presence of AFib, understand its underlying causes, and tailor treatment strategies accordingly.
In summary, the combination of ECGs and blood tests equips us with a powerful toolkit to detect and manage atrial fibrillation. By leveraging these diagnostic techniques, we can demystify the complexities of arrhythmias and take proactive steps toward effective treatment and improved heart health.
Reference: Mayo Clinic. “Atrial Fibrillation Diagnosis.” (2023).
Innovative Therapies and Technologies for Atrial Fibrillation
Cryoablation: Freezing Away Atrial Fibrillation Troubles
In the quest to tame the tumultuous rhythms of atrial fibrillation, a fascinating and innovative therapy has emerged from the realm of modern medicine: cryoablation. This technique, which sounds like something out of a science fiction novel, uses extreme cold to combat arrhythmia atrial fibrillation. But how does this frosty approach work, and what makes it so promising?
Cryoablation is a procedure where extreme cold is applied to specific areas of the heart tissue. The goal is to create small, controlled scars that disrupt the erratic electrical signals causing AFib. Imagine the heart’s electrical pathways as roads, and cryoablation as a strategic roadblock that prevents the chaotic impulses from wreaking havoc.
The process begins with the insertion of a catheter through a blood vessel, usually accessed via the groin, and guided into the heart. Once in position, the tip of the catheter delivers intense cold to the targeted tissue. This freezing effect creates precise lesions that block the abnormal electrical pathways responsible for atrial fibrillation, effectively “resetting” the heart’s rhythm.
Why opt for cryoablation over traditional methods like radiofrequency ablation, which uses heat? One of the key advantages of cryoablation is its precision and safety profile. The freezing technique allows for better control and can reduce the risk of damaging surrounding heart tissue or other crucial structures.
Moreover, cryoablation has shown promising results in treating paroxysmal atrial fibrillation, where episodes are intermittent. Patients often experience a significant reduction in symptoms and an improved quality of life post-procedure. As with any medical intervention, patient selection and individualized care are critical to optimizing outcomes.
While cryoablation is a powerful tool in the fight against atrial fibrillation, it’s not a cure-all. Patients may still require medications to manage their condition or prevent stroke, which remains a risk associated with AFib. However, cryoablation offers a valuable option for those who have not responded well to medication or who prefer a less invasive approach than open-heart surgery.
In the ever-evolving landscape of cardiac care, cryoablation exemplifies how innovative therapies can transform the management of arrhythmia atrial fibrillation. By embracing these advancements, we can offer hope and improved health to those navigating the challenges of AFib.
Reference: European Heart Journal. “Cryoablation for Atrial Fibrillation: Advances and Outcomes.” (2023).